Gabriel Martí-Amengual1, Inmaculada Herrera-Mozo1, Anselmo López-Guillén1,Beatriz Calvo-Cerrada1 , Mikel Uña-Gorospe1,2 and Pere Sanz-Gallen1
1 Department of Medicine. Faculty of Medicine and Health Sciences. University of Barcelona (Spain).
2 ULMA Group. Oñati. Basque Country (Spain).
Gabriel Martí-Amengual. gabrielmarti@ub.edu ORCID: 0000-0002-0316-5260 Inmaculada Herrera-Mozo. herreramozo.i@gmail.com
Anselmo López-Guillén. alopezguillen@gmail.com ORCID: 0000-0002-2462-7567 Beatriz Calvo-Cerrada.beatriz.calvo.cerrada@gmail.com ORCID: 0000-0001-8052-3319 Mikel Uña-Gorospe muna@ulma.com
Pere Sanz-Gallen. 17039psg@comb.cat ORCID: 0000-0001-5592-4014
Abstract
The objective of this work is to provide knowledge about an exceptional case of pulmonary fibrosis related to chronic and high exposure to formaldehyde in a professor of medical anatomy and to review allergic dermatitis with the study of a doctor and a nursing assistant. They were diagnosed with allergic dermatitis to formaldehyde.
Formaldehyde is used to manufacture a large number of industrial products such as urea and melamine phenolic resins, which have various applications in adhesives and binders, wood products such as cellulose pulp for making paper, plastic products, and paints for coatings and products for the textile industry. In other areas, including the clinical field, it is used directly in aqueous solution as a disinfectant, tissue preservative and biocide.
Here, we report three cases of occupational disease caused by exposure to formaldehyde (one case of pulmonary fibrosis and two cases of allergic contact dermatitis). One of the individuals affected worked in a medical school and the other two are employed in university hospitals. The case of pulmonary fibrosis was caused by exposure to high ambient concentrations of formaldehyde in the workplace.
To avoid or minimise cases such as those reported here, health and safety measures must be followed and specific health monitoring should be conducted of exposure to formaldehyde, which is highly sensitising and carcinogenic.
Keywords: formaldehyde, chronic pulmonary fibrosis, contact dermatitis, occupational medicine.
Introduction
Formaldehyde (FA) is a volatile organic compound with a characteristic, irritative odour. Its double bond with oxygen (H2C=O) promotes its reactivity. Formaldehyde is used dissolved in water at a maximum concentration of 40% and is produced on a large scale worldwide. An estimated several million tons per year of this compound are used to manufacture a large number of industrial products including urea and melamine phenolic resins, which have various applications in adhesives and binders, wood products such as cellulose pulp for making paper, plastic products, paints for coatings and products for the textile industry. In other areas, including the clinical field, it is used directly in aqueous solution as a disinfectant, tissue preservative and biocide (IARC, 2012; INHST, 2016).
The concentration of endogenous FA in human blood is about 2-3 mg/l. Exposure of humans, monkeys or rats to FA by inhalation has not been found to alter the concentration of FA in the blood. The average level of formate in the urine of people not occupationally exposed to FA is 12.5 mg/l and varies considerably both within and between individuals (Bolt et al, 2016).
Formaldehyde is mainly retained in the upper respiratory tract, a small part reaches the intermediate airways and only when exposure is high can it reach the terminal bronchioles and alveoli. Lam et al, 2021 perform a meta-analysis on the relationship between asthma and exposure in children and adults and conclude: “The is sufficient evidence of toxicity” for associations between exposure to formaldehyde and asthma diagnosis and
asthma symptoms in both children and adults. Asthma and formaldehyde exposure have also been linked in school students and healthcare workers (Norback et al, 2020; Dumas et al, 2020).
The objective of this work is to provide knowledge about an exceptional case of pulmonary fibrosis related to chronic and high exposure to formaldehyde in a professor of medical anatomy and to review allergic dermatitis with the study of a doctor and a nursing assistant. They were diagnosed with allergic dermatitis to formaldehyde.
Material and Methods
We investigated three individuals working in medical settings, one in a medical school and the other two in university hospitals.
The former is a professor of human anatomy who has been continuously exposed to formaldehyde for some 37 years. He has pulmonary fibrosis. Formaldehyde concentrations were rarely measured in his workplace, but the few measurements taken recorded very high levels.
The two individuals working in university hospitals presented with contact dermatitis. To determine whether this was irritant or allergic, skin tests were performed using the standard test battery of the Spanish Contact Dermatitis and Skin Allergy Research Group (GEIDAC, published by Hervella-Garcés et al., 2016), in addition to other specific tests according to profession and occupational hazards.
Readings were taken at 48 hours (D2) and 96 hours (D4).
The specific tests performed in addition to the standard battery were as follows:
- Rubber additives battery (diaminodiphenylmethane 0.5%, dibenzothiazolyl disulphide (MBTS) 1%, dibutylthiourea 1%, zinc diethyldithiocarbamate 1%, diethylthiourea 1%, 1,3-diphenylguanidine
(DPG) 1%, diphenyl-p-phenylenediamine (DPPD) 1%, diphenylthiourea 1%, 4,4-dihydroxydiphenyl 0.1%, ethylenediamine 1%, ethylene thiourea (imidazolidin thione) 1%, phenyl-beta-naphthylamine
(PBN) 1%, p-phenylenediamine (PPD) 1%, hydroquinone monobenzylether 1%, 2- mercaptobenzimidazole (2-benzimidazole thiol) 1%, mercaptobenzothiazole (MBT) 2%, methenamine (hexamethylenetetramine) 1%, carba mix 3%, mercapto mix 2%, PPD mix 0.6%, thiuram mix 1%, piperazine 1%, tetraethylthiuram disulphide (TETD) 1%,tetramethylthiuram disulphide (TMTD) 1%, ziram (zinc dimethyldithiocarbamate) 1% and phenylisopropyl-p- phenylenediamine (IPPD) 0.1%).
- Antioxidants battery (BHA 2%, BHT 2%, tert-butylhydroquinone 1%, dodecyl gallate 0.3%, octylgallate 0.3%, propyl gallate 0.5% and sodium metabisulphite 1%).
- Other allergens (sodium lauryl sulphate 1%, cocamidopropyl betaine 1%, polyethylene glycol 4%, phenoxyethanol 1%, methyl p-hydroxybenzoate 3%, propyl-p-hydroxybenzoate 3%, EDTA 1%, propylene glycol 2%, sodium benzoate, benzisothiazolinone 0.1% and bronopol 0.5%). (Other isothiazolones: benzisothiazolone 0.1%, octylisothiazolinone 0.025%), isopropyl alcohol (isopropanol) 10%, benzalkonium chloride 0.1%, glycerol 10%, glyceryl monostearate 30%, EDTA 1%, sodium lauryl sulphate 1%, cocamide DEA (coconut diethanolamide) 0.5%, cocamidopropyl betaine 1%, brillant blue (CI 42090) and quinoline yellow (CI 47005) pigments, chlorhexidine digluconate 0.5%, povidone iodine (1/100), monoethanolamine 2%, chloroxylenol 1%, latex 100% and nitrile 100%).
The criteria used to evaluate the results obtained from patch tests at 48 and 96 hours (D2, D4) is show in table I.
Table I. Skin test results interpretation
| Skin reactions | Result |
| No reaction | Negative (-) |
| Erythema with blurred edges | Positive (+) |
| Erythema+Oedema | Positive (++) |
| Erythema+Oedema+vesicles | Positive (III) |
| Not tested | N.T. |
| Non-negative | Irritative (I.R.) |
Results
Below we report three different cases all of them secondary to formaldehyde exposure.
A) Respiratory Disorders
Case 1. Chronic Pulmonary Fibrosis due to formaldehyde. Medical history
A 64-year-old male presented with a history of spontaneous pneumothorax at the age of 18, L1-S1 discopathy and arterial hypertension under treatment; non-smoker, non-drinker with no history of substance abuse; for the last 5 years, presenting with significant dyspnoea on moderate exertion. The pneumology department of a hospital in the Canary Islands diagnosed him with pulmonary fibrosis in July 2020. He is currently awaiting a lung transplant at a hospital in Barcelona.
Employment history
A university professor of anatomy, he has been working for a total of approximately 37 out of 40 years of working life.
He carried out this activity from 1980 to 2020 (the year in which he was declared temporarily unfit to work). He worked at his last university from 1988 to 2020.
His duties as a professor of anatomy included theoretical teaching, practical teaching and research activities. Practical teaching and research activities both involved contact with formaldehyde (preparation of anatomical specimens, teaching of practical classes, dissections for doctoral theses and/or research projects, preparation of samples for histological processing). Formaldehyde exposure is estimated to be about 3 hours/day.
DETERMINATION OF FORMALDEHYDE AT HIS WORKPLACE
Between 1980 and 2000, no measurements of ambient formaldehyde concentrations were performed at his workplace.
In 2001, an assessment of ambient concentrations was requested for the human anatomy practical room (Table II).
This was a large room containing about 10 dissection tables. Several practical groups often worked together there, and there could easily be between 30 and 40 students in the room at the same time (bear in mind that nowadays the number of students in each human anatomy practical group is 25, and that at that time these
that time, the room was used for teaching on degree courses in Medicine, Nursing and Physical Education). The assessment was carried out by the Workplace Health and Safety Office of the Canary Islands Institute of Occupational Safety, a body attached to the Canary Islands Government Department of Employment*.
| Measurement site Formaldehyde concentration (mg/m3) TLV- STEL (mg/m3)** Head of the dissection table: Sample 1 Sample 2 4.705 3.662 0.37 Middle of the dissecting table: Sample 3 4.968 0.37 Bottom of the dissection table: Sample 4 Sample 5 2.158 2.196 0.37 |
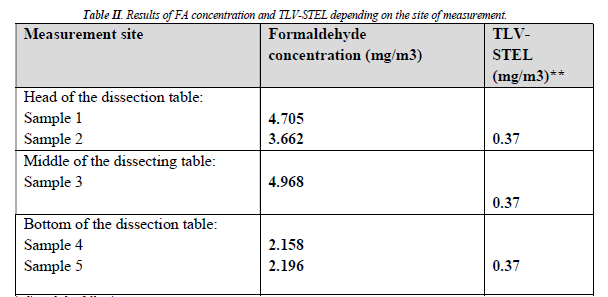
*The report indicated the following: sampling, the simulated conditions did not correspond to real-life conditions, because it is common during practicals to work simultaneously on all the tables, with cadavers impregnated in formaldehyde, which emit much higher concentrations of formaldehyde than those emitted during the present
** Until 2016, Spain did not have a TLV-TWA (time-weighted average exposure for an 8-hour workday, 5 days a week), only a TLV-STEL (short- term exposure for a maximum of 15 minutes).
The university inaugurated new facilities in the 2005-2006 academic year, and new ambient measurements were conducted in November 2006 by the Occupational Risk Prevention Service.
Table III gives the ambient formaldehyde concentrations in the human anatomy dissection room.
Table III. Ambient formaldehyde concentrations as measured by the Occupational Risk Prevention Service (November 2006).
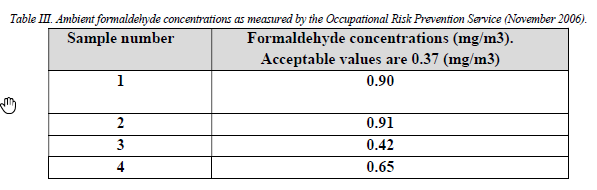
are above the maximum value indicated by the National Institute for Health and Safety at Work (INSHT); consequently, the
immediate cessation of activities involving formaldehyde-fixed material and implementation of preventive measures. In response to this recommendation, human anatomy teaching staff indicated that they would discontinue use of formaldehyde-fixed material and urged the university to implement appropriate protective systems.
In the following years, tables with built-in extraction systems were installed (one per room) and new measurements taken in December 2011 (five years later) found that ambient concentrations of formaldehyde were much lower than in 2006 (from 0.06 ppm in the spaces where no anatomical parts were present in the room, to 0.25-0.46 ppm when formaldehyde-preserved tissue was present in the room).
These latter measurements also found that concentrations in the preservation-storage room remained excessive due to lack of ventilation, with an ambient formaldehyde concentration of 8.66 ppm, where the maximum accepted value is 0.3 ppm.
In February 2022, the professor was granted total permanent disability due to an occupational disease (the various hospitals that he attended ruled out all other possible causes of fibrosis and determined that the most likely cause was chronic exposure to high concentrations of formaldehyde).
B) Skin conditions (allergic dermatitis) Case 2
A 26-year-old male ophthalmology resident, with no medical history of interest, who has been working as a doctor in the ophthalmology department of a university hospital for the past year. In the last two months, he has developed papular and vesicular lesions, with scaling and fissures on both hands accompanied by pruritus. A skin biopsy of the palm of his hand was performed and he was diagnosed with eczematous dermatitis.
Skin tests were performed with readings at 48 hours (D2) and 96 hours (D4).
The results obtained were positive at 48 and 96 hours for: isopropyl alcohol (+) and formaldehyde (+). Isopropyl alcohol is used as a disinfectant and formaldehyde is used sporadically as a preservative for the biopsies performed in the department. The diagnosis is isopropanol and formaldehyde contact dermatitis.
Case 3
A 30-year-old female paediatric nursing assistant who has been working at a university hospital for 11 years. For the last 6 years, she has had isolated episodes of skin lesions on the back of her hands in the form of exanthematous plaques with pruritus; the lesions have resolved after treatment with topical corticosteroids. Over the past few months, her skin lesions have worsened, mainly after using soap in her workplace. This soap contained an antimicrobial agent, bronopol (2-Bromo-2-nitropropanol), which belongs to the group of biocides that release formaldehyde.
The results of the skin tests were as follows:
Positive at 48 and 96 hours for bronopol (+). Positive at 48 and 96 hours for formaldehyde (++).
The diagnosis is formaldehyde and bronopol (formaldehyde-releasing biocide) contact dermatitis.
Discussion
The main route of exposure to formaldehyde is inhalation, and depending on its concentration, exposure to this compound can cause different symptoms. At concentrations of 0.1-5ppm, it can cause eye irritation, tearing and upper respiratory tract irritation and coughing; at concentrations of 5-30ppm, it can cause chest pain, airway irritation, respiratory distress, headache and asthmatic reactions and can aggravate pre-existing respiratory conditions, while at concentrations of 50-100ppm, it can cause pneumonia, pulmonary oedema and even death (Mathur et al., 2007; Saowakon et al., 2015). Permanent exposure to lower concentrations of formaldehyde can produce nasopharyngeal and squamous cell carcinoma in nasal tissues. Genotoxic and mutagenic effects of formaldehyde have been found in various in vitro test systems. As a reactive compound, formaldehyde reacts with nucleic acids and proteins. Results of in vivo studies are more difficult to evaluate. Of particular importance is the question whether cytogenetic effects can only occur as a result of local exposure or also as a result of the systemic availability of formaldehyde (Viegas et al., 2010; Costa et al., 2011; Costa et al., 2013). Bolt et al. (2016) concluded that formaldehyde should be classified as mutagen
The International Agency for Research on Cancer (IARC, 2012) classifies formaldehyde in the group of agents that are carcinogenic to humans (Group 1). Recent meta-analyses have reported a strong association between exposure to this substance and acute myeloid leukaemia (Mundt et al., 2017), while other studies with limited evidence have established a link between formaldehyde and sinus cancer (Zhang et al., 2009).
Formaldehyde is a potent sensitiser and a common cause of allergic contact dermatitis. Patients who are allergic to formaldehyde develop chronic dermatitis that is difficult to manage as the compound is commonplace in the environment and therefore very difficult to avoid. It is widely used as a preservative
because of its antifungal and antibacterial properties, and can be found in cosmetics and household and industrial products (Latorre et al., 2011; Goossens and Aerts, 2022).
The relationship between exposure to formaldehyde fumes and subsequent development of certain respiratory syndromes has been demonstrated in laboratory animals (Peres Leal et al., 2018) and in some occupational settings (Alexardesson and Hedenstierna, 1989). One-year exposure to formaldehyde fumes has been shown to have a cumulative effect leading to alterations in lung function, which may or may not be reversible (Neghab et al., 2011).
If the medical school ad carried out a medical examination of all the human anatomy teaching staff when it became known in 2001 that the concentrations of formaldehyde in the human
ined for subsequent monitoring and identification of changes. Early detection of changes would have helped to avoid or minimise any negative effects on the respiratory tract.
Several studies published in the medical literature have found that exposure to formaldehyde in human anatomy facilities can alter lung function in students and workers, including teaching staff. It has also been found that such alterations in students are reversible (spirometry usually normalises 9-12 months after the cessation of exposure) but that they are persistent in teaching and technical staff (Chia et al., 1992; Ostoji et al., 2006; Abdellah and Nasr El-Din, 2017).
People exposed to formaldehyde have been shown to have a higher incidence of coughing, expectoration, shortness of breath and chest pain than non-exposed subjects. These are symptoms of lower respiratory tract involvement and occur following acute and chronic exposure alike (Akbar et al., 1994).
The effects that prolonged exposure to formaldehyde can have on lung function are summarised in the
function of formaldehyde-exposed workers differed from that of non-exposed workers, we found a clear negative correlation between formaldehyde exposure and lung function in healthy subjects, i.e. formaldehyde exposure has a negative effect on lung function. The formaldehyde-exposed workers included in our study presented a mixed disorder with restrictive and obstructive features. We also found a correlation between lung
In Spain, diseases caused by occupational exposure to formaldehyde, if exposure is proven, are declared as occupational diseases. The problem is that lung diseases are not well defined. Unlike countries like Colombia, which in 2014 expanded the diseases related to occupational exposure to formaldehyde to include chronic respiratory conditions such as chronic bronchiolitis obliterans, chronic pulmonary emphysema, and chronic pulmonary fibrosis (Idrobo-Avila et al., 2017).
The SCOEL recommendation (Bolt et al., 2016) for the working population, adopted in Spanish legislation concerning exposure to formaldehyde, is: 0.3 ppm for time-weighted average exposure for an 8-hour workday, 5 days a week (TLV-TWA) and 0.6 ppm for short-term exposure for a maximum of 15 minutes (TLV-STEL).
Limitations
The main limitation of this study is that there is no follow-up of the environmental concentrations of both the professor of medical anatomy who in 37 years of chronic exposure to formaldehyde there are only three studies of the concentrations of formaldehyde and in all of them they were high. There was also no health surveillance specific to formaldehyde exposure. The two cases of health workers with allergic dermatitis to formaldehyde do not provide studies of exposure to formaldehyde either.
Conclusions
The occupational hazard that led to total disability due to chronic pulmonary fibrosis could have been avoided by improving health and safety measures at work, especially once very high concentrations of formaldehyde had been detected, and in this case, health monitoring specific to occupational exposure to formaldehyde should have been carried out.
The two cases of formaldehyde allergic contact dermatitis would have been more difficult to predict because formaldehyde is present in many areas of everyday life. Nevertheless, when performing their tasks, workers should avoid or minimise contact with sensitising substances such as formaldehyde, and specific health monitoring should also be carried out aimed at early detection of symptoms indicative of formaldehyde exposure.
References
Abdellah RF, Nasr El-Din WA (2017): Pulmonary function parameters among anatomy laboratory workers exposed to formaldehyde. Egyptian Journal of Occupational Medicine 41(3):429-446. https://doi.org/10.21608/EJOM.2017.3931
Akbar KF, Vaquerano MU, Akbar KM, Bisesi MS (1994). Formalehyde exposure, acute pulmonary response and exposure control options in a gross anatomy laboratory. Am J Ind Med 26:61 75. https://doi.org/10.1002/ajim.4700260106
Alexandersson R, Hedenstierna G (1989). Pulmonary function in wood workers exposed to formaldehyde: A prospective study. Arch Environ Health Int J 44:5-11.21.
Bolt HM, Johanson G, Nielsen GD, Papameletiou D, Klein C (2016).SCOEL/REC/125 Formaldehyde Recommendations from Scientific Committee on Occupational Exposure Limits.. 2016-06-30-SCOEL-REC-125-Formaldehyde.pdf (estambiente.it)
Chia SE, Ong CN, Foo S, Lee HP (1992). Medical students exposure to formaldehyde in a gross anatomy dissection laboratory. J Am Coll Health 41:115 9.
Costa, S., Garcia-Leston, J., Coelho, M., Coelho, P., Costa, C., Silva, S., Porto, B., Laffon, B., Teixeira, J. P. (2013).
Cytogenetic and immunological effects associated with occupational formaldehyde exposure. J Toxicol Environ Health A, 76, 217-29.
Costa, S., Pina, C., Coelho, P., Costa, C., Silva, S., Porto, B., Laffon, B. & Teixeira, J. P.( 2011). Occupational exposure to formaldehyde: genotoxic risk evaluation by comet assay and micronucleus test using human peripheral lymphocytes. J Toxicol Environ Health A, 74, 1040 51 https://doi.org/10.1080/15287394.2011.582293
Dumas O, Boggs KM, Quinot C, et al. (2020). Occupational exposure to desinfectants and asthma incidence in US nurses: a prospective cohort study. Am J Ind Med 63(1): 44-50. https://doi.org/10.1002/ajim.23067
Goossens An, Aerts O (2022). Contact allergy to an allergic contact dermatitis from formaldehyde and formaldehyde releasers: A clinical review and update. Contact Dermatitis. 1-8. https://doi:10.1111/cod.14089
Hervella-Garcés M, García-Gavín J, Silvestre-Salvador JF (2016). Actualización de la serie estándar española de pruebas alérgicas de contacto por el Grupo Español de Investigación en Dermatitis de Contacto y Alergia Cutánea (GEIDAC) para 2016. Actas Dermosifiliogr 107 (7): 559-566. http://dx.doi.org/10.1016/j.ad.2016.04.009
(IARC). International Agency for Research on Cancer (2012). Chemical agents and related occupations. Volume 100 F. A review of human carcinogens. Lyon: IARC. https://bit.ly/2DaEsy1.
Idrobo-Avila EH, Vasquez-López A, Vargas-Cañas R. (2017). La exposición ocupacional al formol y la nueva tabla de enfermedades laborales. Rev salud Pública 19(3): 382-385. https://doi.org/10.15446/rsap.v19n3.47740
(INSHT).Instituto Nacional de Seguridad e Higiene en el Trabajo (2016). Formaldehído en la industria de fabricación de tableros. Madrid: INSHT. . https://bit.ly/38sG95n.
Lam J, Koustas E, Sutton P, Padula AM,Cabana MD, Vesterinen H, et al. (2021) Exposure to formaldehyde and asthma outcomes: A systematic review, meta-analysis, and economic assessment. PLoS ONE 16(3): e0248258. https://doi.org/10.1371/journal.pone.0248258
Latorre N, Silvestre JF, Monteagudo AF (2011). Dermatitis de contacto alérgica por formaldehído y liberadores de formaldehído Allergic Contact Dermatitis Caused by Formaldehyde and Formaldehyde Releasers. Actas Dermosifiliogr 102(2):86-97.
Mathur N, Rastogi SK (2007) . Respiratory effects due to occupational exposure to formaldehyde: Systematic review with meta-analysis. Indian J Occup Environ Med 11(1):26-31. http://doi.org/dqfd3k.
Mundt KA, Gallgher AE, Dell LD, Natelson EA, Boffetta P,Gentry PR (2017). Does occupational exposure to formaldehyde cause hematotoxicity and leukemia-specific chromosome changes in cultured myeloid progenitor cells? Crit Rev Toxicol. 47(7):592-602. http://doi.org/d2zx.
Norbäck D, Hashim Z, Ali F, Hashim JH. (2021). Asthma symptoms and respiratory infections in Malaysian students- associations with ethnicity and chemical exposure at home and school. Environmental Research 197:111061. https://doi.org/10.1016/j.envres.2021.111061
Neghab M, Soltanzadeh A, Choobineh A (2011). Respiratory Morbility Induced by Occupational Inhalation Exposure to Formaldehyde. Ind Health 49:89-94.
Ostoji L, Bradari A, Mi K, Ostoji Z, Lovri J, Petrovi P, Ujevi A, Erceg M, Jankovi S, Tocilj J (2006). Pulmonary functions in persons who are professionally exposed to formaldehyde fumes. Coll Antroplol 30 (3) 507-511.
Peres Leal M, Brochetti R, Ignácio A, Saraiva Câmara N, da Palma R, Franco de Oliveira L,Teixeira da Silva D, Santos- Franco A (2018): Effects of formaldehyde exposure on the development of pulmonary fibrosis induced by bleomycin in mice. Toxicology Reports 5: 512 520. https://doi.org/10.1016/j.toxrep.2018.03.016
Saowakon N, Ngernsoungnern P, Watcharavitoon P, Ngernsoungnern A, Kosanlavit R (2015). Formaldehyde exposure in gross anatomy laboratory of Suranaree University of Technology: a comparison of area and personal sampling. Environ Sci Pollut Res Int. 22(23):19002-12. http://doi.org/f72f5f.
Uthiravelu P, Saravanan A, Kishor C, Vaithiyanandane V (2015): Pulmonary function test in formalina expoxed and nonexposed subjects: a comparative study. Journal of Pharmacy and Bioll Science. 7(1):S35-39. https//doi.org/10.4103/0975-7406.155787
Viegas, S., Ladeira, C., Nunes, C., Malta-Vacas, J., Gomes, M., Brito, M., Mendonca, P., Prista, J. (2010). Genotoxic effects in occupational exposure to formaldehyde: A study in anatomy and pathologyformaldehyde-resins production. J Occup Med Toxicol, 5, 25, http://www.occup-med.com/content/5/1/25.
Zhang L, Steinmaus C, Eastmond DA, Xin XK, Smith MT (2009). Formaldehyde exposure and leukemia: A new meta-analysis and potential mechanisms. Mutat Res 681(2-3):150-68. http://doi.org/b2dpfb.